
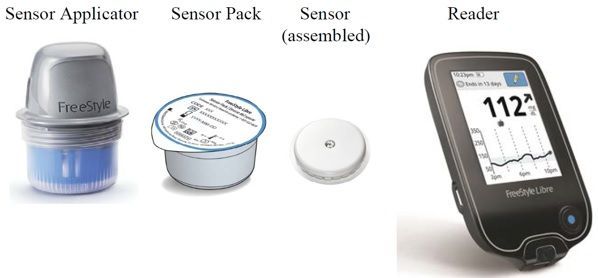
Current prospective randomized studies (NCT03877068 and NCT03508934) are evaluating whether the use of real-time CGM, with an alarm system transmitting glucose values from the patient’s room to the nursing station, can reduce the frequency of clinically significant and severe hypoglycemia events. These studies are in process and will be needed to confirm the accuracy of CGM in the hospital under diverse clinical situations (medicine vs. Because the exact time of collection and sample processing of venous glucose is not correctly documented in the medical records, we did not pair CGM values with those of venous samples. Subsequent studies should aim for larger sample sizes with power to detect differences in low glucose ranges and compare glucose values obtained from CGM to more sophisticated references, such as the Yellow Springs Instrument or by standard laboratory assays. Our study has several limitations, including a small sample size and the low number of hypoglycemic episodes observed. To fill this gap, we are currently testing the use of CGM technology integrated with a telemetry system to alert nurses and providers about downtrending glucose levels (<80 mg/dL) to intervene early and prevent hypoglycemia. These findings are clinically relevant and underlie the potential impact of CGM in hospitalized patients, because improved detection of hypoglycemia in hospitalized patients may facilitate better insulin adjustments and potentially reduce hypoglycemia-related morbidity and mortality. In a recent prospective observational study, we reported that ∼45% of insulin-treated hospitalized patients with glucose <70 mg/dL had asymptomatic hypoglycemia ( 9). In our study, CGM detected nocturnal CGM hypoglycemia (from 2200 to 0600 h) 120 consecutive minutes was detected in 12%. The assessment of nocturnal hypoglycemia and the duration of hypoglycemia events are poorly assessed by POC before meals and bedtime, the current standard of care. Our error grid analyses showed acceptable clinical accuracy, with 98.8% of glucose readings falling into zones A (75.1% n = 1,184) and B (23.7% n = 374). Prior studies in the non–critically ill hospitalized population were performed with previous CGM technology ( 7, 22, 23, 28) requiring capillary glucose for calibration, including Medtronic MiniMed Gold and Medtronic iPro2, reporting up to 91.9–99% ( 7, 22) of values falling into zones A and B of the error grid analysis, respectively. The FreeStyle Libre CGM is a commercially available, factory-calibrated sensor system thus, there is no need for POC BG testing for sensor calibration. In agreement with these studies, we found overall percentages of glucose values within ☑5%/15 mg/dL, ☒0%/20 mg/dL, or ☓0%/30 mg/dL of the POC reference value were 63%, 78%, and 92%, respectively ( 15, 24– 27).
#Freestyle libre flash glucose monitoring sytem pro
In addition, in the pivotal studies of the FreeStyle Libre Pro CGM, an overall 66.5%, 79.4%, and 93.4% of values were within ☑5%/15 mg/dL, ☒0%/20 mg/dL, or ☓0%/30 mg/dL of the capillary glucose reference (FreeStyle Precision Meter), respectively. These values agree with those reported in previous studies, in which the MARD percentage ranged from 11.4% to 14.3% in patients with T1D and T2D. In our study, we found an overall MARD percentage of 14.4%, ranging between 11% and 16% for glucose values between 70 and 250 mg/dL. Institutional Subscriptions and Site Licenses.Special Edition Series: Disrupting Therapeutic Inertia in Diabetes Management.

Special Edition: SGLT2 Inhibitors and Diabetic Kidney Disease.Special Edition Series: SGLT2 Inhibitors in Type 2 Diabetes: Cardiovascular and Renal Outcomes.Special Edition Series: Diabetes and Influenza.



 0 kommentar(er)
0 kommentar(er)
